Restoring Foot Dorsiflexion
Sep 01, 2024Breaking New Ground in Stroke Recovery: Restoring Foot Dorsiflexion and Eversion Through Targeted Exercises
Regaining foot dorsiflexion and eversion after a stroke is a critical milestone in the rehabilitation journey, particularly for those grappling with foot drop—a condition marked by the inability to lift the front part of the foot. This impairment can severely impact gait and overall mobility, making recovery challenging. However, recent advancements in exercise-based interventions are providing hope, showing promise in restoring these crucial movements without relying solely on traditional methods like foot orthoses or functional electrical stimulation (FES) (Bohannon, 2022; Dobkin et al., 2023).
Harnessing the Power of Targeted Exercises
One of the key strategies for improving dorsiflexion and eversion involves targeted exercise regimens designed to strengthen the specific muscles responsible for these movements. The tibialis anterior (TA) and extensor digitorum longus (EDL) muscles play a pivotal role in dorsiflexion, and their coordinated activity is essential for effective walking. Recent research highlights the importance of these muscles working in harmony to achieve the physiological dorsiflexion peak required for proper ambulation (Frigo et al., 2023). This finding underscores the need for stroke rehabilitation programs to incorporate specific strength training exercises aimed at enhancing these muscles' function (Huber et al., 2023).
The Role of Spinal Reflexes in Recovery
Beyond muscle strengthening, spinal cord reflexes also play a crucial role in recovering foot extension and eversion following a stroke. The mechanisms underlying this recovery involve both the intrinsic spinal circuitry and the integration of sensory feedback from the limbs, particularly the feet. Studies have demonstrated that spinal reflexes, such as the H-reflex, can be conditioned to enhance motor function and facilitate the recovery of locomotion after injury (Thompson & Wolpaw, 2023).
Cutaneous afferent inputs from the plantar surface of the foot are particularly significant. These sensory inputs are vital for modulating spinal reflexes and enhancing locomotor patterns. For instance, research has shown that stimulating the plantar surface during the extension phase of movement can promote recovery of stepping in rodent models of incomplete spinal cord injury (SCI), highlighting the importance of sensory feedback in facilitating functional recovery (Fairchild et al., 2010). Similarly, studies emphasize that plantar cutaneous afferents are crucial for normalizing reflex modulation patterns during stepping, suggesting that sensory input is vital for the restoration of locomotion (Knikou et al., 2022).
Leveraging the H-Reflex and Central Pattern Generators
The H-reflex, a spinal reflex analogous to the monosynaptic stretch reflex, has shown particular responsiveness to conditioning protocols. Recent studies have found that operant conditioning of the soleus H-reflex can enhance locomotor function by strengthening the associated muscle activity and restoring symmetrical gait in animal models with incomplete SCI (Thompson et al., 2022). This conditioning promotes beneficial plasticity within the spinal cord, essential for improving motor control and reducing spasticity—a common issue in stroke survivors (Thompson & Wolpaw, 2023). Furthermore, spinal reflex conditioning has been proposed as a therapeutic approach to enhance recovery by targeting specific reflex pathways, thereby promoting broader plasticity that improves overall motor skills (Wolpaw, 2024).
Central pattern generators (CPGs) within the spinal cord also generate rhythmic locomotor patterns. In conjunction with sensory feedback, these neural networks coordinate the sequential activation of leg muscles necessary for locomotion (Rossignol & Frigon, 2011). Recent evidence supports the modulation of reflexes through sensory feedback to enhance the efficacy of the CPG, facilitating more effective locomotion post-injury, particularly in foot extension and eversion (Merlet et al., 2021; Selvanayagam et al., 2023).
Integrating Resistance and Balance Training
Incorporating resistance training into rehabilitation programs has yielded significant improvements in ankle mobility. Exercises involving ankle dorsiflexion against resistance can effectively strengthen the TA and EDL muscles, enhancing dorsiflexion capabilities. Progressive resistance training has been demonstrated to improve overall muscle strength and functional outcomes in stroke patients, contributing to better gait patterns and reducing the incidence of foot drop (Reheem et al., 2022; Kuo et al., 2024). This evidence highlights the potential of exercise interventions to restore mobility and independence in stroke survivors.
Balance training is another critical component of rehabilitation that aids in regaining foot dorsiflexion and eversion. Exercises that challenge balance, such as single-leg stands or dynamic weight shifts, can improve proprioception and stability, which are often compromised in stroke patients (Bastiaanse et al., 2023). By enhancing balance, these exercises indirectly support the recovery of dorsiflexion and eversion, as improved stability allows for more effective movement patterns during walking. Moreover, integrating balance training with strength exercises may provide synergistic benefits, leading to more significant improvements in gait mechanics (Horak et al., 2022).
Functional Exercises and Smart Therapy
Functional exercises that mimic daily activities are essential for promoting the recovery of dorsiflexion and eversion. Activities like step-ups, heel raises, and toe taps can be incorporated into rehabilitation programs to facilitate the use of these movements in real-life contexts. These exercises target the specific muscle groups involved in dorsiflexion and eversion, helping patients practice the coordination and timing necessary for effective gait (Treweek et al., 2023). Functional exercises have been associated with improved walking speed and overall mobility in stroke patients, reinforcing their importance in rehabilitation protocols.
The role of intelligent therapy in enhancing foot function post-stroke cannot be overstated. Stroke rehabilitation experts, personal trainers, and physiotherapists can tailor exercise programs to meet each patient’s specific needs, ensuring that interventions are practical and safe (Dobkin et al., 2023). Techniques such as manual therapy, proprioceptive neuromuscular facilitation (PNF), and neuromuscular re-education can be integrated into exercise regimens further to enhance outcomes (Hebert et al., 2022). These approaches help patients regain voluntary control over their ankle movements, often impaired following a stroke.
Conclusion: A New Hope in Foot and Ankle Recovery for Stroke Survivors
Recent insights into regaining foot dorsiflexion and eversion after a stroke emphasize the transformative power of exercise-based interventions. By focusing on spinal reflexes, targeted muscle strengthening, resistance training, balance exercises, functional activities, and tailored smart therapy, rehabilitation programs can effectively address the challenges posed by foot drop and promote greater independence for stroke survivors. These advances in stroke rehabilitation are not just restoring movement; they are restoring hope (Duncan & Sullivan, 2024).
Arjan Kuipers and Linda Radestad
References:
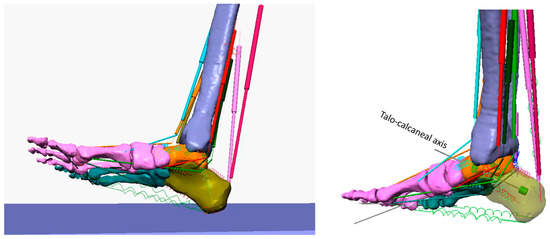
Frigo, C., Merlo, A., Brambilla, C., & Mazzoli, D. (2023). Balanced foot dorsiflexion requires a coordinated activity of the tibialis anterior and the extensor digitorum longus: a musculoskeletal modelling study. Applied Sciences, 13(13), 7984. https://doi.org/10.3390/app13137984
|
Equinus and equinovarus foot deviations (EVFD) are the most frequent lower limb acquired deformities in stroke survivors. We analysed the contribution that the tibialis anterior (TA), extensor digitorum longus (EDL) and plantarflexor muscles play in EVFD via a biomechanical musculoskeletal model of the ankle–foot complex. Our model was composed of 28 bones (connected by either revolute joints or bone surface contacts), 15 ligaments (modelled as non-linear springs), and 10 muscles, modelled as force actuators. Different combinations of muscle contractions were also simulated. Our results demonstrate that, compared to the condition when the foot is suspended off the ground, the contraction of the TA alone produces dorsiflexion (from −18° to 0°) and a greater supination/inversion (from 12° to 30°). The EDL alone produces dorsiflexion (from −18° to −6°), forefoot pronation (25°) and calcaneal eversion (5.6°). Only TA and EDL synergistic action can lead the foot to dorsiflexion suitable for most da
doi.org
|
Khan, M., Ali, S., & Soomro, R. (2021). Role of tissue specific plantar fascia stretching exercises versus myofascial released technique in chronic plantar fasciitis. Journal of Basic & Applied Sciences, 10, 91-95. https://doi.org/10.6000/1927-5129.2014.10.13
Lee, K. and Park, D. (2020). Three-dimensional ankle exercise with combined isotonic technique for an obese subject with plantar fasciitis: a case study. Medicina, 56(4), 190. https://doi.org/10.3390/medicina56040190
Maeshige, N., Uemura, M., Hirasawa, Y., Yoshikawa, Y., Moriguchi, M., Kawabe, N., … & Fujino, H. (2021). Immediate effects of weight-bearing calf stretching on ankle dorsiflexion range of motion and plantar pressure during gait in patients with diabetes mellitus. The International Journal of Lower Extremity Wounds, 22(3), 548-554. https://doi.org/10.1177/15347346211031318
Park, J. (2024). Enhancing post-surgical rehabilitation outcomes in patients with chronic ankle instability: impact of subtalar joint axis balance exercises following arthroscopic modified broström operation. Medicina, 60(2), 328. https://doi.org/10.3390/medicina60020328
|
Background and Objectives: This study aimed to evaluate the effects of subtalar joint axis-based balance exercises on the anterior talofibular ligament (ATFL) thickness, ankle strength, and ankle stability after an arthroscopic modified Broström operation (AMBO) for chronic ankle instability (CAI). Materials and Methods: The study included 47 patients diagnosed with CAI who underwent AMBO and were randomly divided into three groups: control (n = 11), general balance exercise (n = 17), and subtalar joint axis balance exercise (n = 19), regardless of the affected area. Participants in the exercise rehabilitation group performed exercises for 60 min twice a week for six weeks, starting six weeks after AMBO. ATFL thickness, ankle strength, and ankle dynamic stability were measured using musculoskeletal ultrasonography, Biodex, and Y-balance test, respectively, before and after treatment. Results: Compared with the remaining groups, the subtalar joint axis balance exercise group had reduced ATFL thickness (p = 0.
doi.org
|
Reheem, H., Ahmed, W., Mohamed, N., Mohammed, S., & Mohammed, M. (2022). Effect of foot splint and exercises session on foot drop and muscles strengthening among patients with stroke. Egyptian Journal of Health Care, 13(1), 1907-1919. https://doi.org/10.21608/ejhc.2022.249393
Shin, H., Kim, S., Jung, H., Cho, H., & Hahm, S. (2020). Manipulative therapy plus ankle therapeutic exercises for adolescent baseball players with chronic ankle instability: a single-blinded randomized controlled trial. International Journal of Environmental Research and Public Health, 17(14), 4997. https://doi.org/10.3390/ijerph17144997
Zellers, J., Mueller, M., Commean, P., Chen, L., Jeong, H., & Hastings, M. (2020). Multi-system factors associated with metatarsophalangeal joint deformity in individuals with type 2 diabetes. Journal of Clinical Medicine, 9(4), 1012. https://doi.org/10.3390/jcm9041012
Fairchild, M., Kim, S., Iarkov, A., Abbas, J., & Jung, R. (2010). Repetetive hindlimb movement using intermittent adaptive neuromuscular electrical stimulation in an incomplete spinal cord injury rodent model. Experimental Neurology, 223(2), 623-633. https://doi.org/10.1016/j.expneurol.2010.02.011
|
The long-term objective of this work is to understand the mechanisms by which electrical stimulation based movement therapies may harness neural plast…
doi.org
|
Hurteau, M., Thibaudier, Y., Dambreville, C., Chraibi, A., Desrochers, E., Telonio, A., … & Frigon, A. (2017). Nonlinear modulation of cutaneous reflexes with increasing speed of locomotion in spinal cats. Journal of Neuroscience, 37(14), 3896-3912. https://doi.org/10.1523/jneurosci.3042-16.2017
Knikou, M. (2010). Plantar cutaneous afferents normalize the reflex modulation patterns during stepping in chronic human spinal cord injury. Journal of Neurophysiology, 103(3), 1304-1314. https://doi.org/10.1152/jn.00880.2009
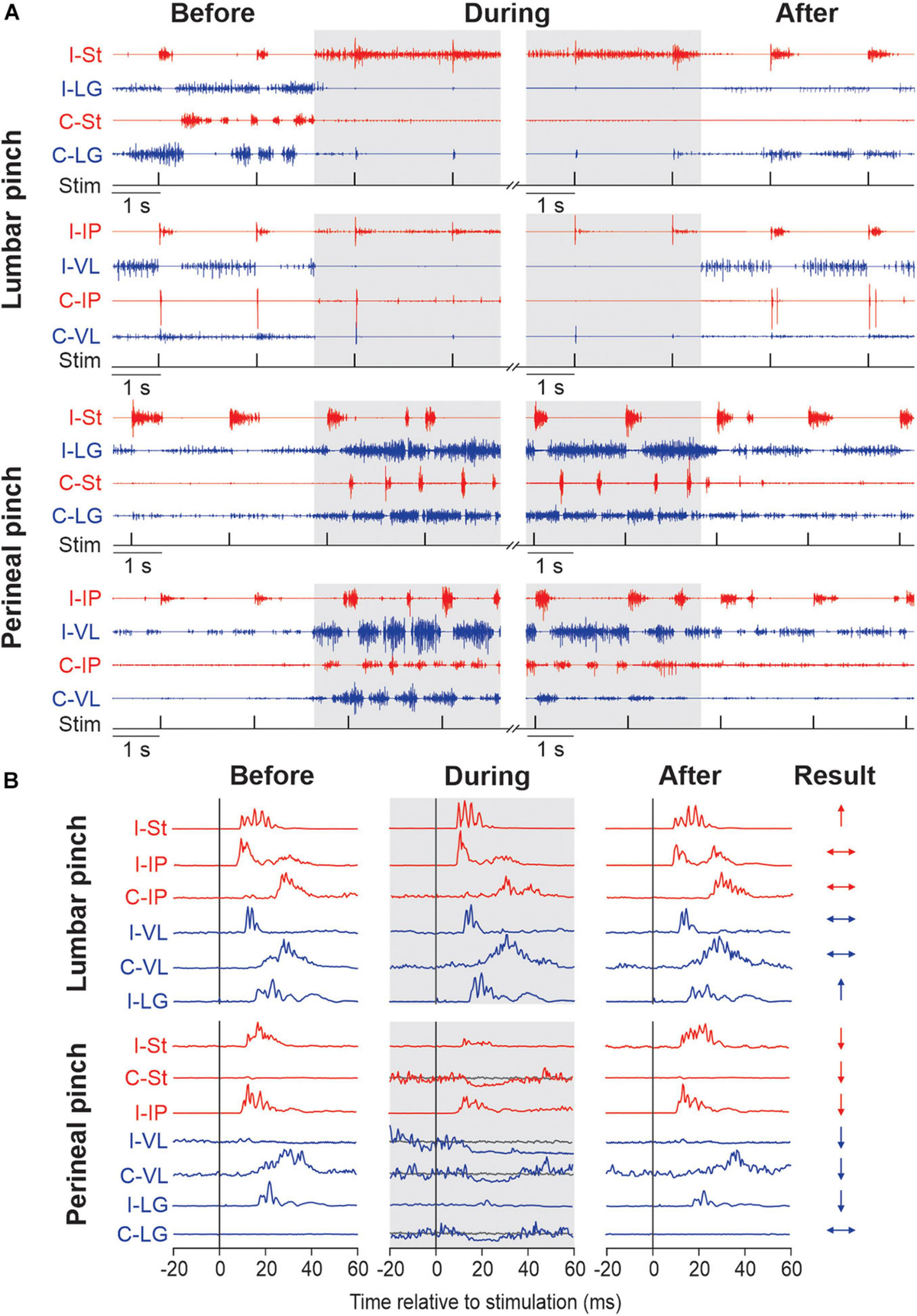
Merlet, A., Harnie, J., & Frigon, A. (2021). Inhibition and facilitation of the spinal locomotor central pattern generator and reflex circuits by somatosensory feedback from the lumbar and perineal regions after spinal cord injury. Frontiers in Neuroscience, 15. https://doi.org/10.3389/fnins.2021.720542
|
Somatosensory feedback from peripheral receptors dynamically interacts with networks located in the spinal cord and brain to control mammalian locomotion. Al...
doi.org
|
Rossignol, S. and Frigon, A. (2011). Recovery of locomotion after spinal cord injury: some facts and mechanisms. Annual Review of Neuroscience, 34(1), 413-440. https://doi.org/10.1146/annurev-neuro-061010-113746
|
After spinal cord injury (SCI), various sensorimotor functions can recover, ranging from simple spinal reflexes to more elaborate motor patterns, such as locomotion. Locomotor recovery after complete spinalization (complete SCI) must depend on the presence of spinal circuitry capable of generating the complex sequential activation of various leg muscles. This is achieved by an intrinsic spinal circuitry, termed the central pattern generator (CPG), working in conjunction with sensory feedback from the legs. After SCI, different changes in cellular and circuit properties occur spontaneously and can be promoted by pharmacological, electrical, or rehabilitation strategies. After partial SCI, hindlimb locomotor recovery can result from regeneration or sprouting of spared pathways, but also from mechanisms observed after complete SCI, namely changes within the intrinsic spinal circuitry and sensory inputs.
doi.org
|
Thompson, A. and Wolpaw, J. (2014). Restoring walking after spinal cord injury. The Neuroscientist, 21(2), 203-215. https://doi.org/10.1177/1073858414527541
Thompson, A., Chen, X., & Wolpaw, J. (2012). Soleus h‐reflex operant conditioning changes the h‐reflex recruitment curve. Muscle & Nerve, 47(4), 539-544. https://doi.org/10.1002/mus.23620
Wolpaw, J. (2014). Spinal reflex conditioning: mechanisms and implications., 209-217. https://doi.org/10.1007/978-3-319-08072-7_39